What is the link between oral infection and joint pain? Bacteria from oral infections can enter the bloodstream, causing inflammation and pain in the joints. This article explains how oral health affects joint health and what steps you can take to manage both.
Key Takeaways
- Oral infections, including gum disease and infected root canals, can trigger autoimmune responses that exacerbate conditions like rheumatoid arthritis (RA) by leading to joint inflammation and pain.
- Individuals with RA are at increased risk for periodontal disease due to factors such as difficulty in maintaining oral hygiene, and the presence of oral bacteria such as P. gingivalis can worsen RA symptoms through a process called citrullination.
- Good oral hygiene practices and regular dental checkups are vital for preventing oral infections and managing RA symptoms, emphasizing the need for a holistic approach to health that considers the interconnection between oral health and systemic conditions.

Introduction
Have you ever considered that the discomfort radiating from your joints might have a starting point somewhere unexpected—like your mouth? Chronic inflammatory diseases, as seen with the film of bacteria that festers on teeth and gums, can extend their impact beyond oral health, potentially leading to tissue damage and inflammation in the joints.
Rheumatoid arthritis (RA), a chronic autoimmune condition notorious for joint pain and inflammation, has been found to have a curious relationship with dental health. Rheumatoid arthritis patients often struggle with regular oral care due to joint pain, which can lead to a cascade of issues, including:
- Dry mouth
- Gum disease
- Tooth decay
- Tooth loss
It is important for individuals with severe RA to prioritize their oral health and work closely with their healthcare providers to manage both their joint symptoms and dental health.
The mouth is a gateway to the body, and its health is integral to our overall well-being. Infected root canals are prime examples of oral infections that can linger unnoticed. Root canal teeth are technically dead and harbor bacteria that can thrive for years without being defeated by the immune system. Why? Because they are protected inside the root canal tooth where there is no blood supply because the tooth is dead and filled with foreign material and tons of bacteria. They can act as a silent source of infection, potentially spreading through the bloodstream to other parts of the body, including joint spaces. Root canal removal is a good idea when it may be the source of systemic inflammation and joint pain. Similarly, gum disease represents another oral infection that can have systemic implications, and loose teeth may be a sign of such issues.
By now, one might wonder how these conditions within the mouth could influence something as distant as joint pain. Bacteria in the mouth do not stay localized; they produce autoantibodies, triggering an immune response. This process, known as citrullination, can mistakenly target proteins within the joints, leading to inflammation and pain. This connection between oral health and joint discomfort is not only fascinating but also crucial for understanding the full scope of autoimmune conditions like RA.
The Role of Oral Bacteria in Inflammation
The oral cavity is home to a myriad of bacteria, some of which play a part in maintaining oral health, while others, when left unchecked, can wreak havoc. Gum disease, oral infections, and periodontal diseases are conditions where harmful oral bacteria thrive, leading to symptoms like tooth pain, fever, and swollen lymph nodes around the jaw. But it’s not just bacterial infections that are concerning; fungal infections like Candida can also establish themselves in the mouth, presenting as white coatings on the tongue or cheeks, complicating the landscape of oral health.
These infections trigger inflammation, a response of the body to fight off these invaders. However, when related to periodontal diseases, this inflammation isn’t contained to just the teeth and gums. It can contribute to the symptoms of rheumatoid arthritis—joint pain and swelling that many people with RA know all too well,.
Good oral hygiene practices are more than just about keeping a bright smile; they’re about managing bacteria and inflammation. Dental abscesses and periodontal infections, if left untreated, can become systemic diseases, affecting far more than just oral health. These conditions underscore the importance of a holistic approach to health that considers the interconnectivity of our body’s systems,.
Periodontal Disease and Rheumatoid Arthritis
Diving deeper into the relationship between periodontal disease and rheumatoid arthritis uncovers startling statistics and a biological underpinning that demands attention. Individuals with RA are twice as likely to suffer from gum disease compared to their counterparts without RA, a clear indication that these conditions are interlinked. The presence of specific bacteria, such as P. gingivalis and Aggregatibacter actinomycetemcomitans, in both periodontal disease and RA, suggests a shared pathogenic pathway that may exacerbate both conditions.
The culprit behind this relationship is a process called citrullination, where proteins are modified in a way that makes them appear foreign to the immune system. This aberrant immune response can lead to the joint lining being attacked, manifesting as the swollen joints characteristic of RA. Moreover, the bacteria from the mouth have been detected in the synovial fluid of joints in people with RA, providing direct evidence of this oral-joint connection.
It’s not just about being more susceptible to periodontal disease if you have RA; the severity of gum disease often mirrors the activity level of RA. Inflammation initiated by severe periodontal disease can precipitate an earlier onset and accelerate the progression of RA. Conversely, treatments like nonsurgical periodontal therapies can reduce inflammation markers, displaying the potential for dental treatment to impact RA management.
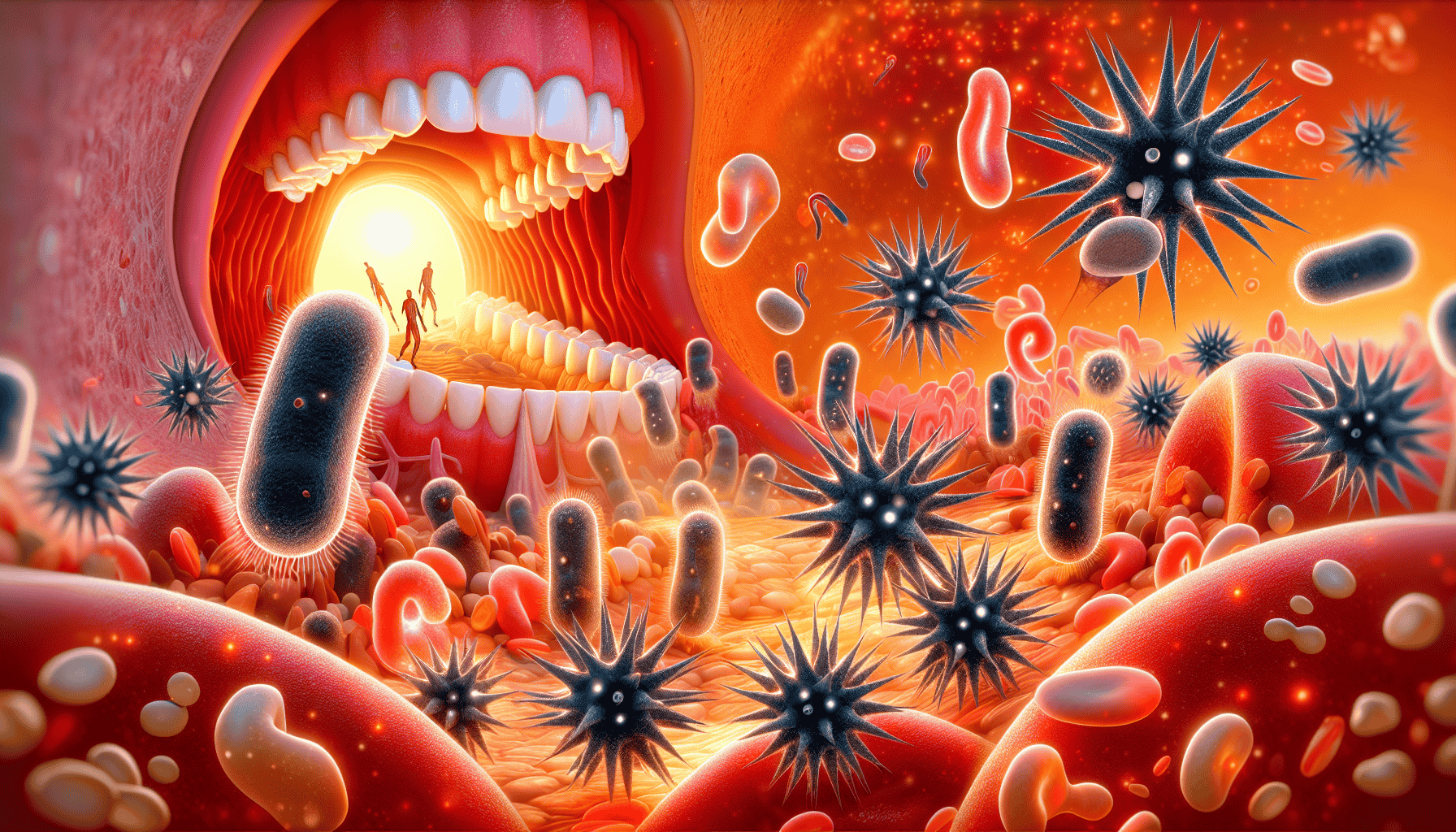
Immune System Response to Oral Infections
The immune system, a complex defense network, is designed to protect us from harm. However, in the case of oral infections, this system can sometimes do more harm than good. Dental infections can trigger the production of autoantibodies, which alter proteins in a way that causes the immune system to attack the joints. When oral bacteria enter the bloodstream, they can infiltrate the synovial fluid, inciting joint inflammation—a painful reality for many with RA.
Aggregatibacter actinomycetemcomitans is particularly insidious due to its ability to induce atypical changes to white blood cells, which are implicated in rheumatoid arthritis. The autoimmune response initiated by periodontitis, another form of gum disease, may set the stage for RA to develop. This link is further reinforced by the formation of immune complexes that can deposit in various organs, contributing to systemic inflammatory reactions.
Good oral hygiene, therefore, is not a mere recommendation; it’s a vital part of preventing infections that could lead to serious complications beyond the mouth. By maintaining a clean mouth, individuals can help their immune system focus on real threats rather than creating unnecessary battles within the body.
Temporomandibular Joint (TMJ) Pain in Arthritis Patients
Turning our attention to the temporomandibular joint (TMJ), we find a striking prevalence of TMJ pain among those with rheumatoid arthritis, ranging from mild discomfort to debilitating pain. About 70% of RA patients experience some degree of TMJ disorder, which can manifest as difficulty opening and closing the mouth due to pain,. While severe TMJ disorder is less common, seen in only 6% of RA patients, its impact on quality of life cannot be overstated.
The prevalence of TMJ disorder in RA patients is higher among females than males, indicating a potential gender-related susceptibility. To assess the extent of TMJ disorders, instruments like the Fonseca Anamnestic Index are employed, allowing physicians to tailor treatments to the patient’s specific symptoms. Factors such as increased body weight have also been associated with a higher risk of TMJ disorders in RA patients, highlighting the multifaceted nature of this condition.
Acknowledging the presence and severity of TMJ pain in arthritis patients is crucial for a comprehensive treatment approach. Addressing this pain is not just about managing symptoms; it’s about improving the overall well-being and functionality of individuals living with RA.
Dry Mouth and Its Impact on Joint Health
Dry mouth, clinically known as xerostomia, is another oral health issue that can have far-reaching effects on individuals with arthritis. Commonly caused by medications such as antihistamines and antidepressants, chronic dry mouth is a frequent complaint among those with RA. Sjogren’s syndrome, an autoimmune disorder often seen alongside RA, significantly increases the risk of chronic dry mouth due to the damage it inflicts on salivary glands.
Some common symptoms of dry mouth include:
- A sticky or dry feeling in the mouth
- Frequent thirst
- Difficulty swallowing or speaking
- A burning sensation in the mouth
- A dry, rough tongue
- Cracked lips
- Bad breath
If you are experiencing chronic dry mouth, it is important to talk to your healthcare provider. They can help determine the underlying cause and recommend appropriate treatment options.
The consequences of dry mouth extend beyond discomfort; it can lead to difficulties in talking, swallowing, and maintaining oral moisture. Moreover, the absence of sufficient saliva production can have a detrimental effect on digestion and dental health, making individuals more prone to cavities and severe oral dryness,.
Thankfully, management strategies for dry mouth exist, such as the use of fluoride rinses and alcohol-free mouthwash, which can mitigate the effects of reduced saliva production. While dry mouth may seem like a minor nuisance, its implications for joint health, particularly in RA patients, demand attention and proactive care.
Preventing Oral Infections to Reduce Joint Pain
Prevention is key when it comes to oral infections and their potential to cause joint pain. Brushing teeth for two minutes twice a day and flossing daily are fundamental practices for maintaining good oral hygiene. For those with arthritis, modifications like using an electric toothbrush or a pre-threaded flosser can make these daily routines more manageable.
Choosing the right oral care products can play a significant role in preventing infections. Here are some recommendations:
- Use fluoride-containing toothpaste to strengthen your teeth and prevent cavities.
- Use a mouth rinse that contains antibacterial properties to kill bacteria and prevent infections.
- Regular dental checkups are equally important, as they allow for the early detection and treatment of any signs of infection.
By following these best practices, individuals can significantly reduce the risk of oral infections, and as a result, may experience a reduction in joint pain associated with RA.
Establishing a consistent oral care routine and visiting a dentist regularly is not just about preserving dental health; it’s a crucial step in managing overall health and mitigating the risks associated with systemic conditions like RA.
Dental Treatment Options for Arthritis Patients
Arthritis patients often require specialized dental treatment options to accommodate their unique needs. For instance, using a bite guard at night can alleviate TMJ symptoms, providing much-needed relief. Similarly, switching to a battery-powered toothbrush with a large grip can help those with joint pain in their hands maintain their oral hygiene without added discomfort.
While dental implants can be a viable option for some, bone growth necessary for implant success can be inhibited in people with RA, necessitating alternative treatment plans. Personalized dental care is essential for arthritis patients, as it allows healthcare providers to develop strategies that address specific symptoms and improve the patient’s quality of life.
A tailored approach to dental care for arthritis patients is not just about treating existing conditions; it’s about preventing future complications and enhancing the overall well-being of those affected by joint pain and inflammation.
Summary
Throughout this exploration of the link between oral health and joint pain, we’ve uncovered the intricate ways in which our body’s systems are interconnected. From the role of oral bacteria in inflammation to the specialized dental care needs of arthritis patients, it’s clear that maintaining good oral health is an integral part of managing rheumatoid arthritis. By staying informed and proactive, individuals with RA can not only safeguard their smiles but also contribute to the overall management of their joint health, potentially reducing pain and enhancing quality of life.
Frequently Asked Questions
How does poor oral health contribute to rheumatoid arthritis?
Poor oral health can contribute to rheumatoid arthritis by leading to periodontal disease, which is associated with harmful bacteria in the mouth that can trigger an immune response and cause inflammation in the joints. This inflammation is typical of rheumatoid arthritis.
Can treating gum disease help manage rheumatoid arthritis symptoms?
Treating gum disease can help manage rheumatoid arthritis symptoms by reducing inflammation markers, potentially alleviating joint pain and swelling. Consider seeking dental treatments like nonsurgical periodontal therapies to help alleviate RA symptoms.
Why is dry mouth a concern for people with rheumatoid arthritis?
Reduced saliva production due to dry mouth increases the risk of oral infections, which can exacerbate joint pain in people with rheumatoid arthritis. This is because saliva contains antibacterial compounds that prevent tooth decay and gum disease.
What accommodations can be made for arthritis patients to improve their dental care routine?
To improve their dental care routine, arthritis patients can use large grip battery-powered toothbrushes and pre-threaded flossers to minimize discomfort, and consider using a bite guard at night to alleviate TMJ symptoms.
Are there any gender differences in the prevalence of TMJ disorders among rheumatoid arthritis patients?
Yes, studies have revealed a higher prevalence of TMJ disorders in female rheumatoid arthritis patients compared to males, indicating a potential gender-related susceptibility to this condition.
 703-712-1053
703-712-1053