If your child is suffering from mouth breathing and pediatric sleep apnea, we have a cure. The treatment for pediatric sleep apnea is to correct the root cause of the problem which is a small obstructed mouth, airway and nasal passageways. Our advanced treatments use specialized orthodontic appliances to increase the space in the mouth, nose and throat to allow for better oxygenation during the day and at night during sleep. By creating more space for airflow and oxygenation, the root cause of kids sleep apnea can be corrected naturally without surgery.

Sleep disorders in children, including sleep apnea, mouth breathing, and night terrors, can profoundly impact their development, behavior, and overall quality of life. The TMJ Sleep and Breathe Center in Vienna Virginia is dedicated to identifying and treating these conditions. We use advanced techniques and therapies to ensure your child achieves a restful, healthy sleep. This comprehensive guide outlines our approach, focusing on palatal expanders, laser frenectomies for tethered oral tissues (TOTs), and myofunctional therapy. The result is truly transformative and addresses the root cause of the obstructive problem.
Why settle for CPAP and unnecessary surgeries such as removal of tonsils and adenoids when a truly natural solution to the cause of the problem is available?
We also offer sleep apnea appliances for adults including the DNA Appliance and other Vivos Devices.
Protocol to Fix Pediatric Sleep Apnea and Mouth Breathing
How we correct the underlying cause of sleep apnea in children. We correct hundreds of airway and sleep apnea problems in children every year. The treatments focus on:
- Correcting tongue posture, so it does not obstruct the airway during sleep
- Increase the size of the mouth and nasal passageway to improve airflow through the entire airway.
- Myofunctional Therapy to correct the function of the tongue and facial muscles.
- Breathing exercises to strengthen the diaphragm in correct breathing muscle patterns.
The Critical Role of Palatal Expanders in Pediatric Sleep Apnea
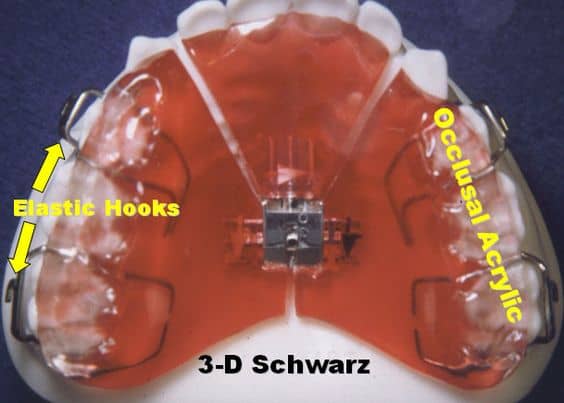
Palatal expanders are devices designed to widen the upper jaw, thereby increasing the size of the mouth and nasal passageways. This widening can have a significant impact on a child’s breathing during sleep, addressing one of the primary physical constraints associated with pediatric sleep apnea. Dental expanders can be designed in many different ways. Expanders can increase nasal breathing by 50%. Nose breathing is one of the primary ways to stop mouth breathing and prevent airway collapse during sleep.
Some of the most popular expanders we use for kids are
How to Cure Sleep Apnea in Children Video
Other Benefits of Sleep Apnea Expanders
By increasing the space in the mouth and nasal passageways, palatal expanders for kids help to promote better alignment of the teeth and jaws. This not only improves breathing but also has lasting benefits for oral health, facial development and a beautiful smile.
Laser Frenectomies: A Light on Tethered Oral Tissues
Tethered Oral Tissues, such as tongue ties, lip ties, and buccal ties, can restrict the movement of facial muscles and the tongue and contribute to breathing and feeding problems, which, in turn, exacerbate sleep apnea symptoms in children.

Laser Frenectomies for Release of Tongue and Lip Ties
Our practice performs laser frenectomy procedures to precisely release TOTs. This minimally invasive procedure releases the ties, significantly improving the child’s ability to breathe, eat, and speak more comfortably. The use of lasers ensures a quick, relatively painless procedure with minimal bleeding and faster healing times.
Myofunctional Therapy: Strengthening for Better Sleep
Myofunctional therapy focuses on strengthening the tongue and other mouth muscles. This therapy teaches children how to properly use these muscles, promoting healthier breathing patterns and correcting mouth breathing, which is often linked to sleep apnea
Beyond immediate improvements in sleep quality, myofunctional therapy offers long-term benefits, including enhanced oral hygiene, better chewing and swallowing functions, and even improvements in speech.
Case Studies: Success Stories from Our Practice
To illustrate the effectiveness of our treatments, let’s explore a few success stories (details modified for privacy):
- Case Study 1: A 7-year-old with severe night terrors and diagnosed with mild sleep apnea showed remarkable improvement after treatment with a palatal expander and myofunctional therapy, experiencing fewer awakenings and deeper sleep.
- Case Study 2: An 8-year-old with a pronounced tongue tie underwent a laser frenectomy, followed by myofunctional therapy. Post-treatment, the child’s snoring decreased, and episodes of apnea were significantly reduced.
These cases underscore the transformative impact of our specialized treatments on children’s sleep health and overall well-being.
Why Choose Us for Your Child’s Sleep Health
The TMJ Sleep and Breathe Center stands at the forefront of treating pediatric sleep disorders with a holistic and innovative approach. We understand the crucial link between oral health and sleep quality and are committed to providing the highest standard of care. Our team is specially trained in the latest techniques to ensure your child receives the best possible treatment in a compassionate, understanding environment.
Night Terrors in Children: Unraveling the Mystery
Night terrors, distinct from nightmares, are episodes of intense fear, screaming, or even running around during sleep, with no memory of the event upon waking. These episodes typically occur in children aged 3 to 12 years and can be distressing for both the child and the parents. Factors like sleep apnea, stress, fatigue, and fever can trigger night terrors. Understanding what night terrors are and recognizing their symptoms can be the first step toward addressing them.
When Do Night Terrors Start?
Night terrors usually start in toddlers and preschoolers, though they can occur at any age during childhood. Recognizing the signs early, such as screaming, intense fear, or flailing while asleep, can help parents seek appropriate interventions.
The Connection Between Mouth Breathing and Sleep Disorders
Mouth breathing in children is often more than just a bad habit—it can be a sign of obstructed nasal airways, enlarged tonsils, or adenoids, contributing to sleep apnea. Chronic mouth breathing can affect facial development, dental health, and sleep quality, leading to conditions like pediatric sleep apnea and night terrors.
Addressing Mouth Breathing and Its Impact
Our practice focuses on treatments that not only address the symptoms of mouth breathing but also tackle the underlying causes. By using palatal expanders to widen the nasal passageway and treating TOTs with laser frenectomies, we can help children breathe more easily through their nose at night, reducing the incidence of mouth breathing and its associated problems.
Mouth breathing can have a negative effect on facial development and profile. Improper breathing patterns put pressure on bone and can change our faces and jaw structure.
Integrating Keywords and Addressing Common Concerns
In addressing these concerns, it’s essential to incorporate the keywords and phrases parents might use when seeking solutions online:
- “How to help with night terrors” and “What causes night terrors in children”: Night terrors in toddlers and older children can often be alleviated by treating associated conditions like sleep apnea. Our comprehensive approach aims to reduce episodes of night terrors by improving overall sleep quality.
- “Signs of sleep apnea in kids” and “Sleep apnea symptoms in kids”: Common signs include heavy breathing while sleeping, cessation of breathing, snoring, and restlessness. Addressing these symptoms early through dental interventions can prevent more serious complications.
- “Pediatric obstructive sleep apnea” and “Can kids have sleep apnea?”: Yes, children can suffer from sleep apnea. Our specialized treatments, such as palatal expanders and myofunctional therapy, are designed to treat pediatric obstructive sleep apnea effectively.
- “What to do if your baby stops breathing while sleeping” and “Sleep apnea in babies symptoms”: Immediate medical attention is critical for any child who stops breathing during sleep. Long-term, addressing potential sleep apnea through early dental evaluation can help prevent such frightening episodes.
Conclusion: A Comprehensive Approach to Pediatric Sleep Health
Our practice’s commitment to addressing pediatric sleep apnea extends to the comprehensive treatment of related conditions like mouth breathing and night terrors. By combining state-of-the-art dental treatments with a deep understanding of sleep health, we aim to improve not just your child’s sleep but their overall well-being and development.
If your child is experiencing any symptoms related to sleep apnea, mouth breathing, or night terrors, we encourage you to reach out to us. Together, we can work towards ensuring your child enjoys the restful, peaceful sleep they deserve, paving the way for a healthy, vibrant future.
Key Takeaways
- Pediatric obstructive sleep apnea (OSA) is a serious condition characterized by repeated upper airway obstruction during sleep, leading to health complications like high blood pressure and behavioral issues if left untreated.
- Diagnosis of pediatric sleep apnea involves clinical evaluation, patient history, physical examination, and confirmation typically using polysomnography (PSG) – the gold standard, although home monitoring studies like oximetry are emerging alternatives.
- Treatment options for pediatric OSA range from surgical interventions like adenotonsillectomy with a high success rate to non-surgical treatments such as CPAP machines and oral appliances, with a collaborative role for dentists in both identifying and treating the disorder.
Demystifying Pediatric Obstructive Sleep Apnea
Pediatric obstructive sleep apnea (OSA) is caused by a partial blockage of the airway during sleep. This condition, not exclusive to adults, underscores the importance of considering obstructive sleep apnea osa in pediatric health as it affects children too.
But what does it look like, and why is it crucial to treat?
Recognizing the Signs: Common Symptoms of Pediatric Sleep Apnea
The signs of pediatric obstructive sleep apnea often include:
- Snoring interspersed with pauses
- Shallow breathing
- Occasional loud snorts or choking sounds as the child regains normal breathing
- Very restless sleep
- Frequently changing sleep positions
- Preferring to sleep propped up on pillows
As a parent, you might observe these signs in your child.
Secondary symptoms during the night may also provide clues. Increased sweating (diaphoresis), bedwetting (enuresis), especially if the child was previously dry at night, or heavy breathing while asleep could all be indicators of pediatric obstructive sleep apnea.
When Breathing Pauses: The Seriousness of Untreated Sleep Apnea
Untreated pediatric sleep apnea can lead to severe health complications. It can cause failure to thrive in infants and young children and increase the risk of developing conditions such as high blood pressure, high cholesterol, prediabetes, and other cardiovascular issues.
Moreover, frequent awakenings or slight brain awakenings due to breathing pauses contribute to poor sleep quality. This lack of quality sleep can result in daytime crankiness and behavioral problems in children. Imagine the challenge of trying to concentrate in school when you’re constantly exhausted. It’s no surprise that untreated sleep apnea can have a significant impact on a child’s daily life.
Evaluating Risk Factors and Causes
There is no one-size-fits-all when it comes to the causes and risk factors of pediatric sleep apnea. It could be due to:
- Enlarged tonsils and adenoids
- Partial narrowing of the airway
- Obesity
- Neuromuscular disorders
- Birth defects affecting facial structure and muscle function
So, how do these factors contribute to sleep apnea?
From Anatomy to Allergy: A Spectrum of Causes
Adenotonsillar hypertrophy, an enlargement of the tonsils and adenoids, is one of the primary anatomical causes of obstructive sleep apnea in children. Beyond the tonsils and adenoids, soft tissue issues at the base of the tongue or in the nose can also play a role. Sometimes, surgical interventions might be necessary to treat these issues.
Moreover, certain facial features such as a small jaw or a flat bridge of the nose may impact airway anatomy and contribute to sleep apnea. Allergies can also exacerbate obstructive sleep apnea by causing swelling or the presence of polyps in the nasal passages, leading to nasal obstruction.
The Path to Diagnosis: Clinical Evaluation and Testing
Diagnosing pediatric obstructive sleep apnea involves a combination of clinical suspicion, patient history, physical findings, and confirmation using polysomnography (PSG) for suspected obstructive sleep apnea cases.
But what do these assessments involve, and are there any alternatives?
Polysomnography: The Gold Standard in Sleep Medicine
Polysomnography, or PSG, is the gold standard in diagnosing obstructive sleep apnea in children. Sleep breathing patterns and oxygen saturation are recorded overnight. This process is involved in assessing sleep quality and potential breathing issues. But it’s not just about breathing. PSG monitors a range of bodily functions such as:
- Brain waves
- Leg movements
- Eye movements
- Oxygen and carbon dioxide levels during the child’s sleep
This is done through sensors attached to the head, face, legs, and body.
In addition to physiological recordings, PSG also includes audio and video monitoring to observe snoring, uncontrolled body movements, or sleepwalking, which provides further insight into a sleep apnea diagnosis.
Alternative Assessment Methods
While PSG is the gold standard, home monitoring studies have advanced and are now producing results comparable to in-lab polysomnography. Oximetry is one such home diagnostic test for pediatric sleep apnea, which monitors and records oxygen levels throughout the night.
If oximetry indicates a risk of obstructive sleep apnea in a child, recommendations for further sleep apnea testing may follow. This means that even if in-lab polysomnography is not immediately accessible, there are still valid alternatives for diagnosing sleep apnea.
Innovative Treatment Options
Once a child has been diagnosed with sleep apnea, what’s next? Fortunately, emerging research and innovative treatment options for pediatric sleep apnea, such as surgical interventions and CPAP machines, underscore the importance of early intervention to reduce long-term risks.
Surgery: When It’s Necessary and What It Involves
Adenotonsillectomy and other surgical interventions are often discussed as treatment options for pediatric sleep apnea. This procedure, commonly referred to as T and A, dramatically improves obstructive sleep apnea in children, particularly in cases with massive tonsils that obstruct airways.
The success rate of adenotonsillectomy in treating childhood sleep apnea is approximately 85%. However, like any surgical procedure, adenotonsillectomy carries risks. In a clinical trial, 2.7% of children experienced a serious adverse event related to the procedure. Therefore, it’s crucial to discuss all options and potential risks with your healthcare provider.
Non-Surgical Therapies: Oral Appliances and More
Non-surgical treatments for pediatric sleep apnea include oral appliance therapy, CPAP machines, and lifestyle changes. These alternatives are particularly relevant for those who are hesitant about surgery or for whom surgery is not an option. CPAP therapy, for example, is a first-line treatment for adult sleep apnea and is considered a second-line therapy for children, with improvements noted in symptoms and quality of life.
A dentist can provide customized oral appliances, such as mouthguards, which push the lower jaw forward to maintain an open airway in cases of mild to moderate obstructive sleep apnea. For obese children, weight loss and a healthy diet are recommended as part of the treatment plan.
The Role of Dentistry in Treating Pediatric Sleep Disorders
Dentists play a key role in identifying sleep-disordered breathing in children by observing tonsil size during oral examinations and referring patients for further assessment. They can also provide oral appliances, such as mouthguards, that have become increasingly popular in the treatment of pediatric obstructive sleep apnea and mouth breathing.
Beyond Teeth: How Dentists Aid in Sleep Apnea Management
Dentists can:
- Identify symptoms of pediatric obstructive sleep apnea
- Recognize conditions such as adenotonsillar hypertrophy
- Act as gatekeepers in the early identification of children with adenotonsillar hypertrophy, referring them to specialists for further evaluation and diagnosis.
Dentists not only play a crucial role in diagnosing sleep apnea but also in treating it. They can provide oral appliances and have an increasing awareness and involvement in managing these conditions.
Orthodontic Interventions: Palatal Expanders and Other Dental Devices
Orthodontic interventions can be incredibly helpful in managing pediatric sleep apnea. One such intervention is the use of a palatal expander, which is designed to gradually widen the upper jaw, increasing the size of the nasal cavity and potentially reducing obstructive events during sleep.
Other dental devices, such as mandibular advancement devices, can reposition the lower jaw and tongue, decreasing the likelihood of airway obstruction. These orthodontic treatments ensure that the dental device suits the unique anatomy and needs of the child, enabling more effective management of their sleep apnea symptoms.
Navigating Life with Pediatric Sleep Apnea
Parents can prevent serious health conditions in children with sleep apnea, a type of sleep disorder, by ensuring they receive effective treatment. This includes adopting a worry box technique to help their child articulate and set aside their concerns before sleep, and starting bedtime routines earlier for additional comfort.
Adjusting room lighting to be neither too dark nor too bright helps create a sleep environment that is comfortable for children with sleep apnea. Clearing pathways and securing exterior doors is also important to reduce sleepwalking incidents.
A consistent and healthy bedtime routine is beneficial in signaling to children with sleep apnea that it’s time for sleep.
Summary
Pediatric sleep apnea is a serious condition that requires awareness, understanding, and action. It’s crucial to recognize the symptoms, understand the causes, and be aware of the diagnostic procedures and treatment options. Whether through surgery, non-surgical therapies, or lifestyle changes, effective treatment can significantly improve a child’s quality of life and prevent long-term health complications. Remember, early intervention is key.
Frequently Asked Questions
What are some common symptoms of pediatric obstructive sleep apnea?
Common symptoms of pediatric obstructive sleep apnea include snoring interrupted by pauses, shallow breathing, very restless sleep, increased sweating, and bedwetting. These signs may indicate the presence of the condition.
What are the consequences of untreated pediatric sleep apnea?
Untreated pediatric sleep apnea can lead to serious health issues such as failure to thrive, high blood pressure, and behavioral problems due to poor sleep quality. It’s important to seek treatment to avoid these consequences.
Untreated pediatric sleep apnea can lead to serious health issues such as failure to thrive, high blood pressure, and behavioral problems due to poor sleep quality. It’s important to seek treatment to avoid these consequences.
Some causes and risk factors of pediatric sleep apnea include enlarged tonsils and adenoids, partial narrowing of the airway, obesity, and certain neuromuscular disorders or birth defects affecting facial structure and muscle function. These factors can contribute to the development of sleep apnea in children.
What are some treatment options for pediatric sleep apnea?
Treatment options for pediatric sleep apnea include surgical interventions like adenotonsillectomy, non-surgical therapies like oral appliances and CPAP machines, as well as lifestyle changes such as weight loss and a healthy diet. These options aim to improve breathing during sleep and alleviate symptoms.
How can dentists assist in managing pediatric sleep apnea?
Dentists can assist in managing pediatric sleep apnea by identifying symptoms, referring patients for assessment, and providing oral appliances to help manage the condition. It’s an essential role in ensuring comprehensive care for pediatric patients with sleep apnea.
 703-712-1053
703-712-1053